Additional Roles Team
A key feature of PCNs is the introduction of Additional Roles. The Additional Roles Team will help to build a sustainable future for the PCN. Kingfisher PCN is in the process of recruiting extra specialist clinical staff to provide holistic, patient-centred care. For 2023/24, Kingfisher PCN has selected the following roles to join the Additional Roles Team:
Clinical Pharmacists
For the provision of specialist medication and lifestyle advice. Clinical Pharmacists will be able to perform medication reviews and advise of any changes needed to your prescription. They may be involved in monitoring your long-term illness. They will become key members of a multi-professional Care Home Team who will be responsible for the provision of enhanced health in Care Homes. The ambition will be to expand upon this and introduce a multi-professional service for patients within their own homes.
First Contact Physiotherapists
First Contact Physiotherapists (FCPs) are highly skilled practitioners with specialist knowledge of musculoskeletal (MSK) problems. They will be able to help you with mechanical pain through timely interventions including exercise, lifestyle advice, and pain management.
Pharmacy Technicians
Pharmacy Technicians undertake specific projects to promote the safety and quality of prescribing across the PCN. They will contact patients to carry out checks and offer advice and guidance on matters concerning medications. Pharmacy Technicians will also be a key part of the Care Home Team.
Physician Associates
Physician Associates (PAs) are healthcare professionals who help provide care for patients. Physician Associates always work under the direct supervision of a named GP.
PAs can take a medical history, perform examinations and diagnose patients with a wide range of health problems. While PAs currently do not have prescribing rights, they can prepare prescriptions for GPs to review and issue.
Social Prescribers
Social Prescribers are able to assist with non-medical problems by identifying needs and finding solutions by putting the patient in touch with the most appropriate organisation to help. Social Prescribers have a firm understanding of the range of options and local services available to patients. This may include signposting to community groups or voluntary workers.
Care Coordinators
Care Coordinators will build and sustain the smooth running of the Additional Roles Team – coordinating calendars and securing access for patients across our 6 practices. Care Coordinators will also have an important role in the introduction of the Care Home Team – coordinating Multidisciplinary Team Meetings (MDTs) for Kingfisher Care Homes.

Meet The Team

Erin Fenton
Physician Associate
Jamie Farmer
Safeguarding Coordinator

Nicola Hinton
Social Prescriber

Rachel Durman
Clinical Pharmacist Lead

Norman Davey
Care Coordinator

Kayleigh Neade
Social Prescriber

Sherree Salter
Care Coordinator Lead

Henna Zulfiqar
Physician Associate

Joanne Dixon
Care Coordinator

Jason Siluvaimani
First Contact Physiotherapist Lead

Keerthana Muthurajan
First Contact Physiotherapist

Chianne McGowran
Care Co-Ordinator

Tricia Pridding
Social Prescribing

Natalie Gilliland
Digital Transformation Lead

Irfan Sattar
First Contact Physiotherapist

Clare Potter
Physician Associate Lead

Karolina Syczyk
Physician Associate

Lucy Vesmanis
Physician Associate

Sahima Ali
Clinical Pharmacist
Sophie Smith
Clinical Pharmacist
Lisa Clapham
clinical Pharmacist
What will the Kingfisher PCN Additional Roles Team do?
There are 7 National Service specifications that we are expected to deliver:
- Structured medication reviews (ensuring all medication remains appropriate and safe).
- Enhanced health in care homes (including regular reviews of care home residents).
- Anticipatory care (working proactively alongside community teams to offer greater support to those considered at high risk).
- Supporting early cancer diagnosis (promoting screening and ensuring early referral and identification of cancer where possible).
- Personalised care (shared decision making and encouraging self-management).
- Prevention and diagnosis of cardiovascular disease (such as heart attacks and stroke).
- Locally agreed actions to tackle inequalities.
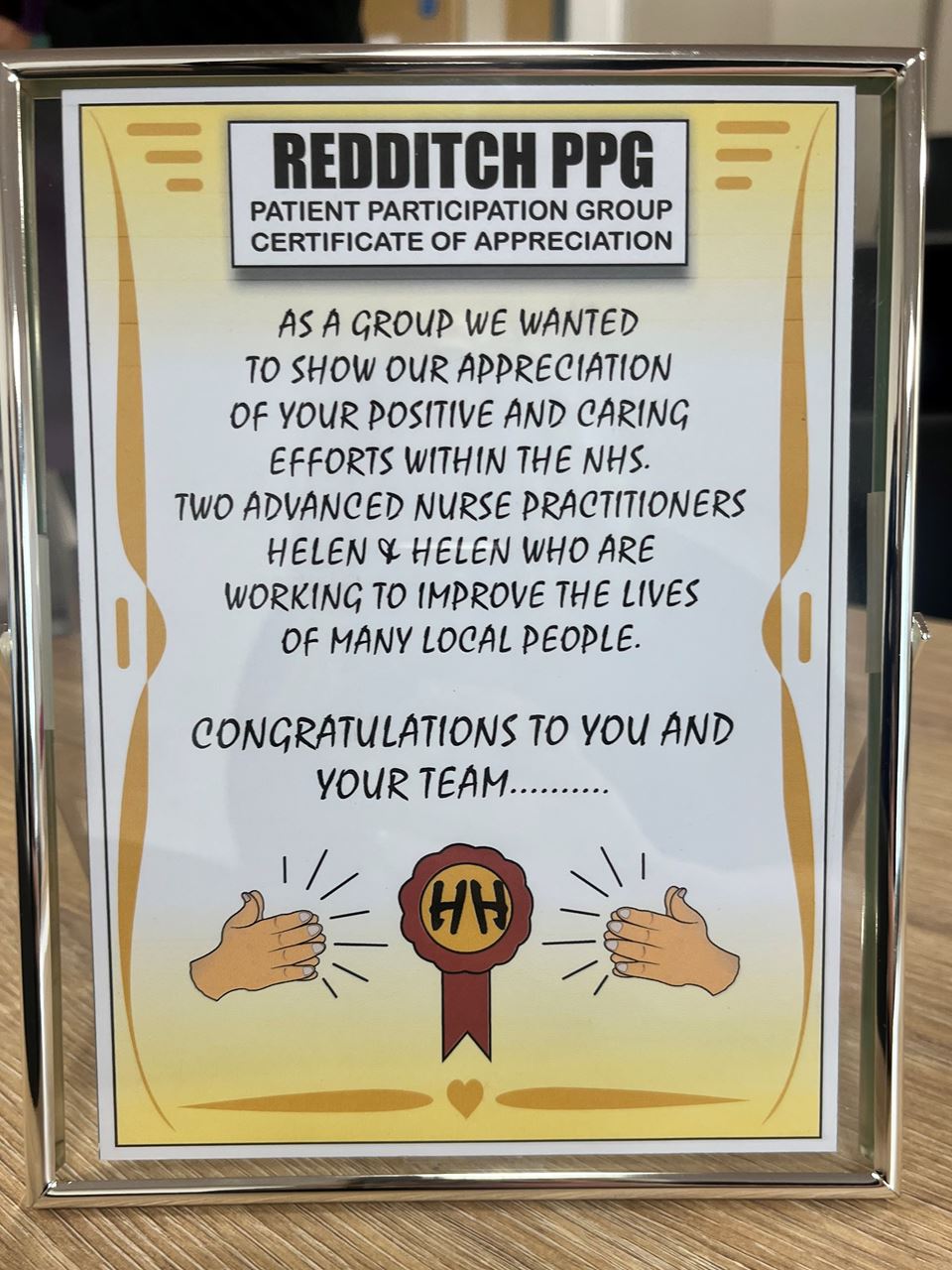
Frailty Team
The Frailty Team are working collaboratively within the community providing comprehensive personalised care to residents of care homes and nursing homes with an aspiration that this will develop into providing this service for residents still living at home. The aim of the service is to move away from traditional reactive models of care to a service providing proactive management plans for residents with complex care needs.
The Frailty Team has been live since November 2021.

Helen Abdullah
ACP Lead
Frailty Team

Helen Smith
ACP
Frailty Team

Helen Clay
Nurse
Frailty Team

Julia Griffiths
Care Coordinator
Frailty Team